Hidradenitis Suppurativa is a chronic, common and painful inflammatory skin disease affecting approximately 1% of the population. Onset occurs after puberty, and the condition is most active during the early twenties to late thirties. Less commonly HS occurs into the 40s and 50s. HS skin lesions occur in the underarms (axillae), groin, and less commonly on the buttocks and abdomen. HS skin lesions are painful, deep-seated nodules, papules and abscesses, leading to suppuration (formation or discharge of pus), fibrosis, distortion and scarring of the skin in affected areas. The cause of HS is not known, but studies are ongoing.
Underarm involvement has no gender predilection whereas genital and inner thigh lesions are significantly more common in women. Perianal, perineal and buttock lesions tend to be more common in men. One or several sites may be involved at the same time or at different times in the same person. HS is not well known to non-dermatology physicians. This may cause delay in the diagnosis and treatment. Failure to recognize HS and give a correct diagnosis and advice on how to manage this chronic disease adds to patients’ severe distress and impaired quality of life.
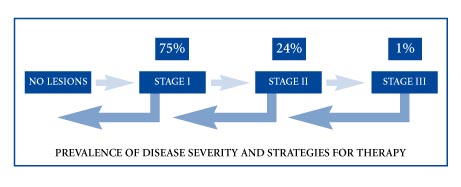
(Table from: Hidradenitis Suppurativa Foundation, Inc. www.hs-foundation.org)
There is no one treatment that is beneficial for all cases of HS; the treatment of HS is challenging. The goal of treatment is to reduce the extent and progression of the condition. Stage I HS is characterized by tender red nodules and early sinus tracts that are separated from each other. Sometimes topical and short-course systemic treatments are beneficial in Stage I. In Stage II these nodules and sinus tracts become linked to each other by tunnels and thickened scar tissue. In Stage II, medical and surgical therapies are available, including local excision, oral anti-inflammatory medications (tetracyclines, dapsone), anti-androgen therapies (spironolactone, drospirenone, oral contraceptive pills), and “intralesional” injection of anti-inflammatory steroid locally into the skin nodules (kenalog). These treatment options are usually combined. If these approaches are not helpful, biologic injectable drugs (adalimumab, etanercept, infliximab) may be considered on a case by case basis. These biologic drugs suppress specific immune system functions that cause HS (as a side effect, these drugs can increase the risk for certain infections). In very difficult HS cases, the oral steroid (prednisone) can be added on a short term basis while other therapies begin to work more completely. Stage III disease is characterized by the development of large, painful areas of abscess, sinus tracts and fibrous tissue that drain (suppurate) chronically. For Stage III HS, wide and deep excision surgery may be beneficial. For Stage III HS, medical treatment may be only palliative (it may only reduce the severity of outbreaks). Biologic drug therapies, intralesional steroid and short courses of low-dose prednisone are used in combination in Stage III HS when surgery is not the chosen approach (and sometimes even in patients that have previously undergone surgery).
There is no evidence that HS results from a lack of hygiene, yet these views often cause those affected by HS to suffer in silence. Tobacco smoking and weight gain do not cause HS; however, they can cause HS to be more serious and prolonged (last later into a person’s lifetime). It is reasonable for physicians to advocate weight loss and smoking cessation in HS sufferers.

Reference: Thoracodorsal Artery Perforator Flap for the Treatment of the Axillary Hidradenitis Suppurativa. Sebahattin Kandal, MD, Suhan Ayhan, MD, Yakup Sariguney, MD, Serhan Tuncer, MD, and Fulya Findikcioglu, MD.

Before and after treatment with infliximab. Reference: Mekkes and Bos, Br J Dermatol 2008; 158: 370–4.